The Emergency In The UK Emergency Services
Britain still promises emergency response but can no longer deliver it. Ambulance waits are 92 minutes. Fire deaths up 21% in a year. They share a single cause: the state retained legal duty while dismantling operational capacity. Promises have met pavement.

Picture an ambulance crew at three o'clock on a Wednesday afternoon, parked outside an emergency department in a provincial English town. The patient—a stroke victim—lies in the back. The paramedics have been there for ninety minutes. They cannot leave. They cannot hand over. The emergency department has no beds, no staff to receive the patient, no physical space to accommodate another trolley.
Meanwhile, seven miles away, a cardiac arrest call comes through. The nearest available unit is twenty-three minutes out. Not because the ambulance service lacks vehicles. Not because paramedics are idle. But because three crews are immobilised outside the same hospital, waiting for a system downstream to absorb the patients they have already collected.
This is not an operational hiccup. This is standard.
The A&E Queue Is The Real Emergency Service
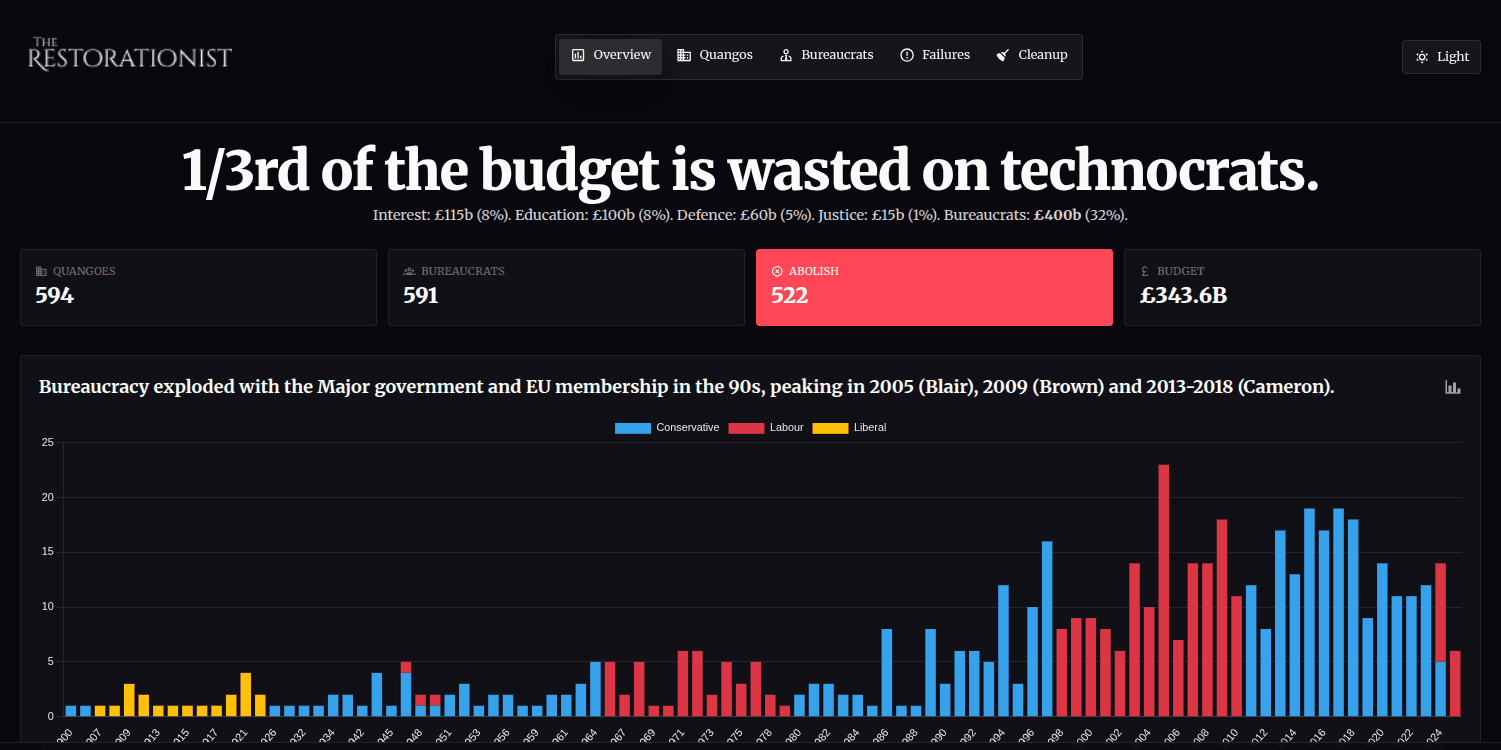
In December 2022, Category 2 ambulance responses—heart attacks, strokes, serious injuries requiring urgent attention—averaged one hour and thirty-two minutes nationally. The constitutional target is eighteen minutes. At the system's breaking point, the state was delivering emergency care five times slower than its own published standard. Category 1 calls, the most life-threatening emergencies where every second compounds the risk of death or permanent injury, averaged ten minutes and fifty-seven seconds against a seven-minute target.
These are not outliers. These are averages. Half of all responses were slower still.
Britain's ambulance services are failing, but the failure point is not on the road. It sits in the handover queue, where emergency medicine transforms into a waiting game. Every minute a crew spends trapped outside an ED is a minute stolen from the next emergency. The public experiences slow response times. The operational reality is hospitals have become bottlenecks, and ambulances have become mobile storage units for a jammed system.
Response time targets remain formally intact on paper. In practice, NHS operational planning guidance for 2025/26 sets a socialist "interim objective" for Category 2 responses: average no more than thirty minutes. Not eighteen. Thirty. This is not a winter surge adjustment. This is permanent policy-level concession the state can no longer meet standards it wrote into constitutional documents barely a decade ago.
Even this degraded interim target is being missed. Across the eleven ambulance trusts in England, only five met the thirty-minute standard in 2024/25. The national average was thirty-five minutes and twenty-two seconds. But the national average conceals a fractured system. Across integrated care system areas, Category 2 response times ranged from twenty-one minutes and forty-three seconds to one hour, one minute, and fifty-seven seconds.
Read those numbers again. In some parts of England, if you have a stroke, the ambulance arrives in just over twenty minutes. In others, you wait more than an hour.
This is not variation. This is systemic fragmentation, where your chance of survival depends less on medical science and more on postcode lottery.
The Handover Chokepoint
The NHS Standard Contract for 2024/25 sets out ambitions for ambulance handover times: all handovers within sixty minutes, ninety-five percent within thirty minutes, sixty-five percent within fifteen minutes. The word "ambition" is doing heavy work here. These are not targets. They are aspirations, carefully worded to avoid the accountability targets would impose.
The reality: more than one in four handovers in 2024/25 were delayed thirty minutes or longer. Over twenty-five percent of every patient collected by an ambulance spent at least half an hour waiting outside a hospital before transfer could occur. Many waited far longer. The data does not capture the distribution of delays beyond the threshold, but operational reports describe waits of multiple hours as routine during pressure periods.
Every delayed handover cascades. Three ambulances queued outside one emergency department means three crews unavailable for the next cardiac arrest, the next road traffic collision, the next overdose. The system's actual "response time" is increasingly determined not by how quickly ambulances can reach patients, but by how quickly hospitals can absorb them. Dispatch performance becomes irrelevant when crews cannot offload.
Estimates suggest millions of ambulance hours are lost annually to handover delays. The equivalent of thousands of paramedics have been removed from active service—not through redundancy, but through immobilisation. Over a thousand patients per day are potentially exposed to increased harm risk due to delayed care. This is not mismanagement. This is a capacity deadlock between ambulance services and hospitals, and both institutions are trapped in it.
The important fact is not the individual horror story. It is the systemic drift. Policy documents no longer discuss recovery to the eighteen-minute constitutional standard. They discuss "more realistic" interim standards of thirty minutes. The state has quietly conceded it cannot meet its own design assumptions, so it is redesigning the assumptions instead while leaving the constitutional language untouched. The gap between what the law promises and what the system delivers widens every year.
Changing What Counts When You Cannot Increase What Matters
Call volumes to ambulance services have risen from 8.2 million incidents annually to 8.8 million. The system's response has not been to increase physical capacity. It has been to change how incidents are counted and managed.
Telephone triage systems—"hear and treat"—now resolve a significant proportion of calls without dispatching a vehicle. Reclassification of call categories has quietly downgraded incidents previously considered emergencies into something less urgent on paper. Both measures produce headline improvements in published statistics. Neither reduces the number of physical emergencies requiring hospital conveyance. Neither shortens the time crews spend queuing outside emergency departments. Neither addresses the throughput bottleneck killing people in the back of stationary ambulances.
This creates a statistical illusion. The dashboard shows improvement. The ground shows deterioration. It is not a lie, exactly. It is a substitution of measurement for reality, and it has become the preferred method of managing a system the state technocrats can no longer afford to operate properly.
The Commons Library summary of winter 2022/23 describes "record waiting times." Subsequent winters showed improvement from that catastrophic baseline but targets continued to be missed for most measures through winter 2024/25. The language here is revealing: improvement measured not against the target, but against the worst-ever recorded performance. Very clever, Sir Humphrey.
The standard has shifted from "meeting constitutional requirements" to "better than the absolute nadir."
The Engineered Absence of Slack
The deeper problem is slack, or rather its complete removal. Emergency systems require spare capacity: extra crews, open beds, the ability to absorb spikes in demand without collapsing into gridlock. Britain has spent two decades systematically removing slack from emergency services in pursuit of efficiency.
Lean staffing models. "Just in time" bed occupancy targets optimising hospital capacity to run at maximum theoretical throughput. Chronic social care bottlenecks preventing discharge of patients who no longer need acute beds but have nowhere else to go. High sickness and attrition rates under sustained pressure because the system operates continuously at breaking point.
What remains is a system with no margin for error. Every winter surge, every norovirus outbreak, every summer heatwave, every bad weekend becomes a near-fatal shock. The resilience has been optimised out. An emergency service designed to run efficiently cannot run at all when efficiency means zero tolerance for variance.
A resilient emergency service does not run "efficiently" in the management consultant sense. It runs with margin. It maintains spare capacity specifically for the purpose of absorbing unpredictable demand spikes without degrading performance. Victorian fire brigades understood this. Modern hospital trusts, operating under efficiency targets set by Treasury models, do not.
The result is visible in the data. When demand rises even moderately, the entire system lurches toward crisis. When demand spikes severely, as in December 2022, response times blow out to five times the constitutional standard. There is no shock absorber. There is no reserve capacity. There is only the queue, lengthening inexorably.
When Duty Meets Operational Impossibility
Ambulance staff are not simply tired. They are experiencing something clinically distinct: moral injury. This occurs when professionals are forced by systemic failure to act against their training, their ethics, and their purpose.
Paramedics report being unable to respond to cardiac arrests because their vehicle is stuck in a queue outside an emergency department. They describe leaving patients untreated for hours not through negligence but through sheer impossibility—there is nowhere to take them, no capacity to receive them, no pathway through the bottleneck. They work shifts where operational control is lost entirely, where the pretense of emergency response gives way to crisis management of the crisis management system itself.
Industrial action, particularly in Northern Ireland, has surfaced what had previously been managed through quiet attrition: chronic understaffing, poor retention, unsustainable workloads. This is a human bottleneck layered on top of a structural one. You cannot recruit your way out of a system design flaw. You cannot train your way past a capacity deficit. The workforce is not the problem. The workforce is the canary, and it has been singing warnings for years while management published dashboards showing green.
Research and coronial reports increasingly link delayed ambulance responses to deterioration or death in time-critical conditions: cardiac arrest, stroke, sepsis, trauma. The phrase "no evidence of harm"—a favourite of managerial deflection—no longer survives contact with reality. The evidence exists. It accumulates in coronial files and clinical audits and bereaved families' testimony. It is simply inconvenient to the statistical performance management framework being maintained at policy level.
Delay is not a KPI miss. Delay is a clinical risk. And the system is now structured to produce delay as its default output.
Fire & Rescue Has Become General Response
While ambulances queue outside hospitals, fire services face a different manifestation of the same structural failure: expanding responsibilities without expanding capacity, rising demand without rising throughput, legal duties piled on top of existing obligations without the operational muscle to discharge them.
In the year ending June 2025, fire and rescue services in England attended 628,764 total incidents. This represents a five-point-seven percent increase on the previous year and a twenty-five percent increase over ten years. The growth is not evenly distributed across incident types. Non-fire incidents—road traffic collisions, medical emergencies, rescues, flooding—rose sixty-eight percent over the decade, from 126,491 incidents to 212,726.
Fire services have quietly become the emergency capacity backstop for a failing state infrastructure. When ambulances cannot respond quickly enough, fire crews are dispatched to medical emergencies. When flooding overwhelms local capacity, fire services fill the gap. When road traffic collisions require extrication, fire and rescue attends.
The mission has expanded from fire suppression to general emergency response without corresponding expansion in resources, staffing, or equipment budgets.
"Collaborating incidents"—where fire and rescue services attend alongside other emergency services—have more than trebled over the decade, from approximately 21,400 in the year ending June 2015 to 73,962 in the year ending June 2025. This is not fire services choosing to expand their remit. This is fire services being pressed into service to cover gaps in ambulance capacity, police response, and local authority emergency planning.
Meanwhile, fires themselves spiked sharply year-on-year in the most recent dataset. Total fires attended rose twenty-eight percent from 129,638 to 165,697. Secondary fires—outdoor fires, vehicle fires, rubbish fires—jumped forty-eight percent year-on-year to 98,687. Whether this represents an actual increase in fire incidents or improved reporting is unclear from the published data, but the operational impact is identical: more callouts, more deployments, more strain on finite crew availability.
Response times are drifting upward. The drift is measured in seconds, which makes it easy to dismiss. This would be a mistake. In emergency response, small average changes in seconds can conceal dangerous increases in the tail of the distribution—the worst ten percent of responses where delays compound into fatalities.
Average total response times for primary fires reached nine minutes and fourteen seconds in the year ending June 2025, up twelve seconds year-on-year and thirty-seven seconds compared to a decade ago. For dwelling fires specifically, average response time was eight minutes and ten seconds, up nine seconds year-on-year and twenty-two seconds over ten years.
These are averages. They tell you nothing about the worst cases, the rural responses, the responses delayed by multiple simultaneous incidents, the responses slowed by traffic or equipment failures or crew unavailability. The average hides the variance, and in emergency services, variance kills.
Fatalities Rising While The System Drifts
Fire-related fatalities in England for the year ending June 2025: 279 deaths. This is up from 231 the previous year, a twenty-one percent increase. Fatal fires rose seventeen percent from 218 to 255. Non-fatal casualties increased six-point-one percent from 6,268 to 6,650.
These numbers do not speak for themselves. They require context. Fire deaths in Britain had been trending downward for decades, the result of improved building standards, widespread smoke alarm installation, public safety campaigns, and professional fire service capacity.
The recent increase could be statistical noise—fatality data is volatile year-to-year because the absolute numbers are mercifully small. Or it could be the leading edge of systemic degradation, the first visible symptom of delayed responses and overstretched capacity beginning to show up in mortality statistics.
What cannot be disputed is the direction of travel. Demand is rising. Response times are lengthening. Fatalities have spiked. The system is under strain, and strain shows up eventually in outcomes.
After Grenfell, Laws Without Machinery
The Grenfell Tower fire killed seventy-two people in June 2017. In response, bureaucrats passed the Fire Safety Act 2021 and the Building Safety Act 2022, established more regulatory frameworks, imposed more compliance duties on building owners and managers, created another quango in the Building Safety Regulator, and commissioned a public inquiry producing multiple interim reports and thousands of pages of recommendations.
Notice the technocrat response to tragedy.
- More regulation will look like activity.
- More compliance duties will provide a legal disclaimer.
- Another quango will pass the problem to someone else.
- A public inquiry will stop the plebs from rioting.
What the state conspicuously did not do was rebuild the inspection capacity, enforcement muscle, or professional accountability systems required to make those laws effective at scale.
Fire protection enforcement actions across England increased twenty-four-point-one percent from 17,177 in 2018/19 to 21,323 in 2024/25. This is the headline number suggesting improvement.
The reality beneath it is more complex. HMICFRS—His Majesty's Inspectorate of Constabulary and Fire & Rescue Services—reports in its State of Fire and Rescue 2024-25 assessment protection staff remain under "considerable strain" due to competing demands: inspections, consultations, enforcement actions, implementation of Grenfell Inquiry recommendations, involvement in building remediation programmes.
The proportion of fire services meeting targets for auditing high-risk buildings rose from 21.6 percent (eight out of thirty-seven services) in 2021/22 to 36.6 percent (fifteen out of forty-one services) in 2024/25. This is improvement.
It is also evidence sixty-three-point-four percent of fire services are still failing to meet their own targets for inspecting the buildings most likely to kill people in bulk if they catch fire.
Laws expanded. Duties multiplied. Operational headroom did not. The state announced reforms, published strategies, and declared victory. The machinery required to execute those reforms remained under-resourced, fragmented, and increasingly unable to keep pace with the workload created by the legislation.
Regulated On Paper, Unaccountable In Practice
Fire risk assessors, the professionals tasked with evaluating whether buildings are safe, remain lightly regulated, inconsistently accredited, and largely unpoliced. Professional competence varies wildly. Box-ticking compliance is endemic.
There is no effective deterrent against incompetence because there is no effective enforcement mechanism to impose consequences on assessors who produce inadequate work.
The state has outsourced responsibility for fire safety to a market in compliance services without building the oversight architecture to ensure the market produces actual safety rather than paperwork.
A building can be "compliant" on paper—risk assessment completed, signed off, filed with the responsible person—and lethally dangerous in practice, because the gap between the two is occupied by variable professional standards, inconsistent enforcement, and accountability so diffused nobody can be definitively blamed when things go wrong.
This story should now be familiar across every government department. It's a deliberate, obstinate pattern across every single domain.
The state retains legal obligation, political responsibility, and moral authority. It has quietly shed the operational capacity needed to discharge any of them. The result is a fire safety regime where compliance is measured by the existence of documents, not by actual reduction in fire risk.
The bureaucrats are fighting fire by filling in forms, because that's all they know.
Responsibility Everywhere, Accountability Nowhere
Fire safety enforcement in Britain is split across local fire and rescue services, local authority building control bodies, the absurd Health and Safety Executive, and the toothless Building Safety Regulator. Each has specific statutory duties. None owns the entire risk. No unified enforcement strategy exists across these bodies. Responsibility dissolves into process.
Fire brigades report insufficient protection staff to conduct regular inspections of high-risk buildings. Enforcement is reactive and complaint-led rather than systematic and proactive. Services lack capacity to revisit buildings on a planned cycle. Instead, they respond to referrals, complaints, and incidents, arriving after problems have already developed rather than preventing them through regular oversight.
This fragmentation is not accidental. It is the accumulated result of successive reforms, each designed to clarify responsibilities and improve coordination, each adding another layer of complexity without simplifying the underlying structure. When failure occurs, each node in the system can point to compliance with its own narrow remit.
- The building owner followed the risk assessment.
- The risk assessor followed the guidance.
- The fire service responded to complaints.
- The local authority processed the building control paperwork.
- The regulator issued notices.
Everyone did their job. The building burned anyway. Very clever, Sir Humphrey.
This is a governance design flaw, not a regulatory gap. Adding another regulator, another code of practice, another layer of oversight does not solve it. It makes it worse, increasing the surface area of responsibility while further diffusing accountability. What is missing is not rules. Britain has rules in abundance. What is missing is someone visibly on the hook for measurable outcomes, with genuine personal and professional downside for failure. And no politician technocrat wants that jeopardising his next job in Brussels.
Liability Divorced From Control
Post-Grenfell remediation has shifted costs onto leaseholders, created years-long delays, and left unsafe buildings occupied while legal and financial disputes drag on. This is not a policy accident. It is a perverse incentive engine operating exactly as designed by a system optimised to avoid difficult decisions about who pays.
Leaseholders are paying for remediation they did not cause and cannot control. Building owners and managing agents control the remediation process but do not bear immediate financial pain. Insurers and lenders tighten terms, freezing the property market for affected buildings. Safety work becomes a legal and financial contest, not an urgent operational duty.
The result is moral hazard at industrial scale.
Responsibility without authority. Risk without agency. Safety deferred by process. The system has created conditions where the economically rational behaviour for many actors is delay, dispute, and deflection—precisely the opposite of what post-Grenfell reform was supposed to achieve.
Thousands of buildings identified as requiring remediation remain unremediated years after assessment. Residents live in homes they cannot sell, cannot mortgage, cannot afford to remedy, and cannot safely remain in if fire breaks out.
The state created legal liability for the problem. It did not create a mechanism to solve the problem quickly. So the problem persists while lawyers argue and costs escalate and the buildings remain occupied and dangerous.
This is not a "we need clearer guidance" problem. This is a liability correspondence problem.
The people carrying the risk are not the people making decisions. The people making decisions are not the people paying costs. Nobody has both authority and incentive to act urgently. So nothing happens quickly, and unsafe buildings remain occupied while the state congratulates itself on having passed laws and established regulators.
Paper Systems Replacing Operational Muscle
The ambulance crisis and the fire safety crisis are not separate phenomena. They are the same failure mode, expressed in different domains.
Britain has retained statutory responsibility for emergency response and public safety. It has published targets, strategies, frameworks, and legislation in abundance. It has conducted inquiries, issued recommendations, announced reforms, created regulators, and updated building codes.
What it has not done is maintain the operational capacity—the staffing, the physical infrastructure, the enforcement machinery, the system slack—required to deliver on any of it.
Ambulance services have constitutional targets of eighteen minutes for Category 2 responses. Actual performance hit ninety-two minutes at peak. The interim target is now thirty minutes. The national average is thirty-five minutes. In some areas it exceeds sixty minutes. More than a quarter of handovers are delayed beyond thirty minutes.
The system cannot do what it claims to do.
Fire services have laws requiring regular inspection of high-risk buildings. Sixty-three percent of services fail to meet their own inspection targets. Protection staff are under considerable strain. Response times drift upward year by year. Fatalities rose twenty-one percent in the most recent annual data.
The system cannot do what it claims to do.
Both systems have substituted statistical management for physical throughput, measurement for capability, policy documents for actual muscle. Both announce improvements while performance deteriorates. Both publish compliance rates while outcomes worsen. Both operate under expanding legal duties while capacity remains static or declines.
This is not austerity in the traditional sense. Austerity implies temporary fiscal restraint pending economic recovery. This is institutional atrophy: the slow-burn erosion of state capacity while formal structures remain intact.
The laws are still on the books. The targets are still published. The responsibilities are still legally assigned. The state simply cannot do what it says it will do, and it has learned to manage this gap through redefinition, reclassification, and carefully worded "interim objectives" rather than rebuilding.
The failure is distributed, technical, slow-burn, and hard to dramatise. There is no single villain. There is no sudden collapse. Just a widening chasm between what the system claims to be and what it can actually deliver when tested by reality. The ambulance waits. The building burns. The statistics improve on paper. The bodies accumulate in coronial files.
We Do Not Need More Regulation
The solution is not another regulator, another code of practice, another compliance framework, another inquiry producing another thousand-page report with another hundred recommendations. Britain is drowning in rules. What it lacks is consequences, throughput, and accountability that bites.
- Make handover times a hard metric operational failure, not a "pressure indicator" managed through dashboard colours. Publish them by hospital trust, monthly, in league table form. Not buried in annual reports. Not aggregated nationally. Trust by trust, month by month, unavoidable and comparable. If handover delays exceed thirty minutes for more than twenty-five percent of patients for three consecutive months, the trust chief executive explains to the public in a press conference why they have failed and what specific actions with specific deadlines will fix it.
- Do the same for high-risk building remediation. Publish completion rates by local area. Name the buildings. Name the responsible persons. Name the enforcement bodies. If a building identified as high-risk remains unremediated twelve months after formal notice, someone's name appears beside it in the public record with an explanation of why. Not a consultation. Not a strategy. An explanation of who is responsible for the delay and what consequences they face.
- Assign outcome owners. Not committees. Not working groups. Not partnerships or collaboration boards or multi-agency steering groups. Single accountable entities with the duty to deliver measurable results and genuine personal and professional downside for failure. An NHS trust does not have collective responsibility for handover delays. A named executive has individual responsibility. A local authority does not have collective responsibility for building safety enforcement. A named officer has individual responsibility.
- Strip the ideological nonsense from the discussion. This is not complicated. This is a throughput problem. This is a liability problem. This is an incentive problem. This is a slack problem. These are mechanical diagnoses with mechanical solutions, and they do not require new theories of governance or innovative regulatory frameworks. They require the state to do what it already claims to do: enforce its own laws, maintain its own systems, and hold people accountable when things go catastrophically wrong.
- Rebuild slack. Emergency services require spare capacity by design. Stop optimising for efficiency and start designing for resilience. Maintain beds above the theoretical minimum. Staff crews above the calculated minimum. Hold back reserve capacity specifically for surge absorption. This costs money. It appears wasteful on spreadsheets during quiet periods. It is the difference between a system degrading gracefully under pressure and a system collapsing into ninety-two-minute response times when demand spikes.
- Simplify ownership. Every high-risk building should have one entity responsible for its safety, with clear legal liability and no ability to pass the buck through complex ownership structures or management contracts. Every hospital should have one accountable individual responsible for handover throughput, with career consequences for sustained failure. Fragmentation is the enemy of accountability. Consolidate responsibility until it cannot hide.
The Victorian Standard We Have Abandoned
Britain's Victorian emergency services were built with slack and visible accountability. Fire brigades maintained spare capacity explicitly for surge response. Hospitals operated with margin. Building regulations were enforced by inspectors with real authority and professional pride. When systems failed, the responsible parties were identifiable and faced consequences—public censure, professional ruin, criminal liability where negligence was proven.
Modern Britain has inverted this model.
We have built systems designed to avoid consequences. Accountability is distributed to the point of invisibility. Responsibility is outsourced to paperwork. Capacity is optimised away in pursuit of efficiency metrics that look impressive in Treasury models but collapse under real-world variance.
The Victorians built Chadwick's sanitation reforms, Bazalgette's sewers, professional fire brigades, hospital systems. They built with massive over-capacity relative to immediate need because they understood infrastructure exists to handle peaks, not averages.
They built accountability into professional structures—engineers signed their work, inspectors faced ruin for corruption, officials were personally liable for negligence.
We have inherited their physical infrastructure and allowed it to decay. We have inherited their institutional models and hollowed them out. We announce reforms and publish strategies while the gap between promise and delivery widens every year. The Victorians would be baffled by a state apparatus capable of producing compliance documents but incapable of guaranteeing a stroke victim receives medical attention within an hour of calling for help.
The Clock Is Running
The British state is still – apparently, in places – capable of building things. It built a vaccine rollout programme in months during COVID-19. It built Nightingale hospitals. It can, when sufficiently motivated by immediate political pressure, execute at speed and scale. What it appears to have lost is the will to maintain, the ability to enforce, and the nerve to assign blame.
Emergency services are failing because the state has become comfortable announcing responsibility without bearing it, setting targets without funding them, passing laws without building enforcement capacity, and managing crises through redefinition rather than resolution. This is not political opinion. This is observable fact, documented in response time data, fatality statistics, inspection compliance rates, coronial reports, and the growing chasm between what the law requires and what actually happens on the ground.
Category 2 ambulance responses hit ninety-two minutes at peak. The interim target is now thirty minutes instead of the constitutional eighteen. The national average is thirty-five. In some areas it exceeds sixty. More than one in four handovers are delayed beyond thirty minutes. Fire deaths rose twenty-one percent year-on-year. Sixty-three percent of fire services fail to meet high-risk building inspection targets. Response times drift upward. Demand rises. Capacity remains static.
The numbers do not lie. The system is failing, measurably and documentably, in ways that kill people.
Britain once built emergency services with margin, with muscle, with consequences for failure. We can do so again. It requires political will, not regulatory innovation. It requires rebuilding capacity, not redefining targets. It requires making accountability real, visible, and costly to ignore. It requires accepting emergency services cannot be optimised for efficiency without sacrificing resilience. It requires someone in authority saying out loud the state has failed and here is how we will fix it, with names attached to deliverables and deadlines attached to consequences.
The alternative is what we have now: a state apparatus hollowed out to the point of decorative functionality, where emergency response is increasingly a matter of postcode lottery rather than system design, and where the gap between constitutional promise and operational delivery widens every year while officials publish dashboards showing green and congratulate themselves on meeting interim objectives nobody voted for.
The ambulance outside the emergency department is still waiting. Ninety minutes now. The patient's condition deteriorates. The next cardiac arrest goes unanswered. The unsafe building remains occupied. The statistics improve on paper through careful categorisation. The fatalities accumulate. The system grinds on, producing compliance documents and missing targets and explaining away failure through references to unprecedented demand and complex partnerships and challenging circumstances.
The clock is running. People are dying. The state knows the numbers. It publishes them, buries them in reports, explains them away, and then publishes more strategies. At some point the public will notice the gap between what they were promised and what they receive has become unbridgeable through words alone. At some point the legitimacy of a state apparatus declaring itself responsible for emergency response while demonstrably incapable of delivering it will crack.
We are not there yet. But the distance closes every time an ambulance idles outside a hospital for two hours. Every time a fire crew cannot reach a dwelling fire in under ten minutes. Every time an unsafe building sits unremediated years after formal notice. Every time someone dies because the system designed to save them has been optimised into paralysis.
The Victorians built for peaks. We optimised for averages. They built margin. We removed slack. They assigned accountability. We distributed responsibility. They measured outcomes. We measure compliance. They faced consequences. We publish strategies.
The choice is simple. Rebuild capacity, restore slack, impose accountability, and accept emergency services require over-provision by design. Or continue managing decline through statistical redefinition while the gap between promise and performance becomes a chasm, and the public begins to understand the state can no longer do what it claims.
The numbers are already there. The evidence is already published. The failure is already documented. What remains is whether anyone in authority has the nerve to acknowledge it, own it, and fix it before the next Grenfell, before the next winter of record ambulance delays, before the preventable deaths pile up past the point where dashboards and interim objectives can explain them away.
The ambulance is still waiting. The clock is still running. And every minute of delay is another minute closer to the point where the gap between what Britain promises its citizens and what Britain can actually deliver becomes impossible to deny.